About
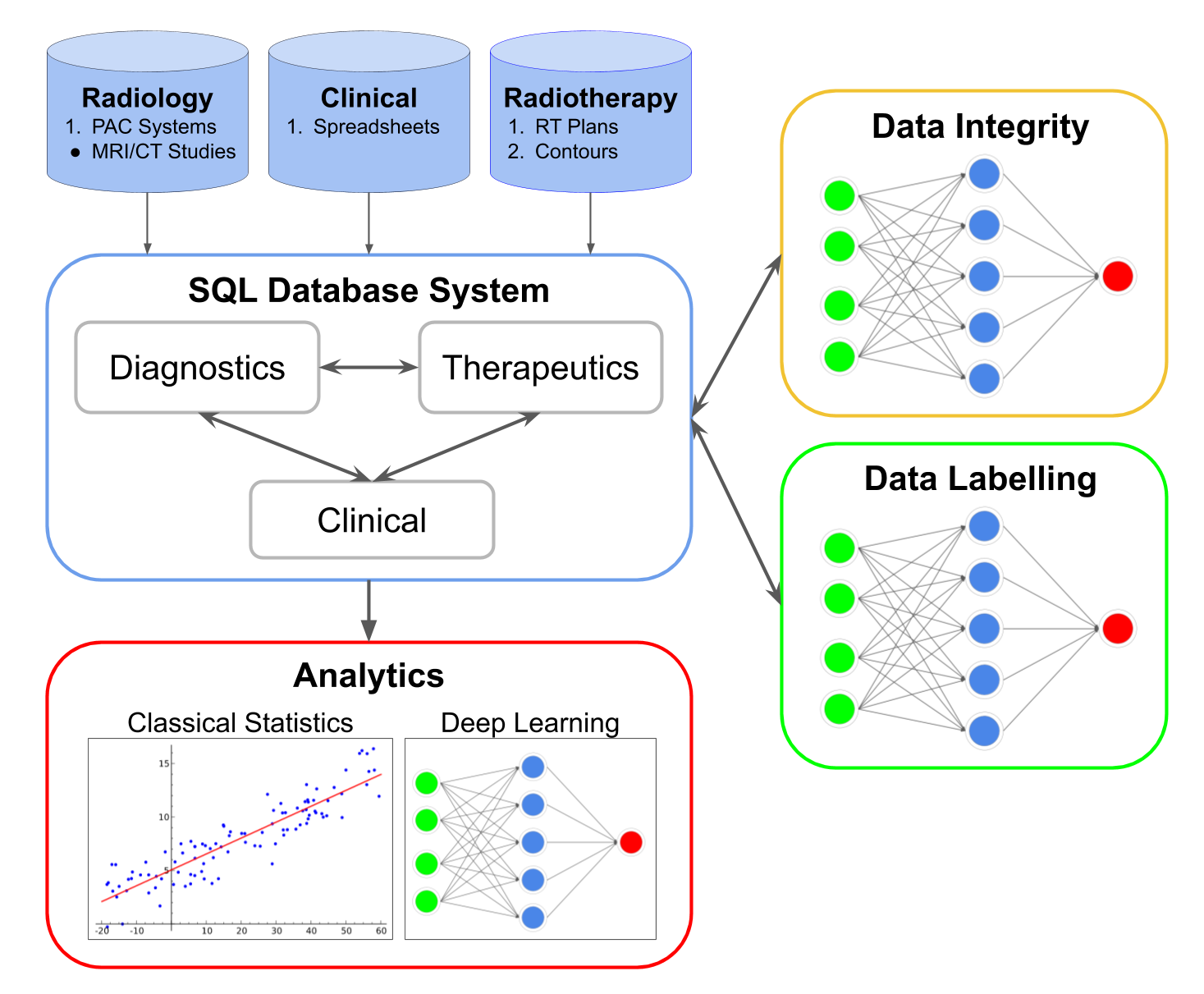
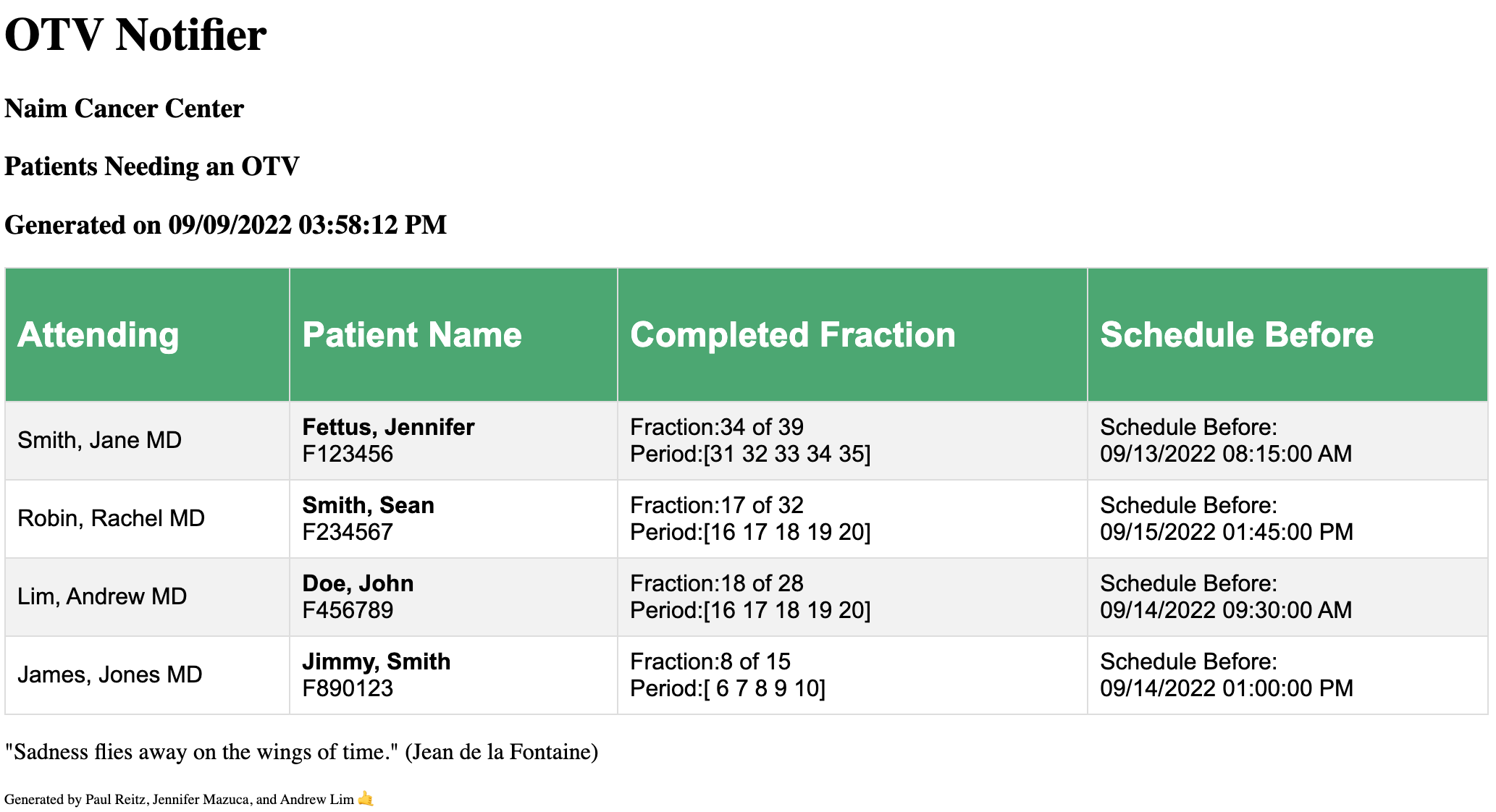
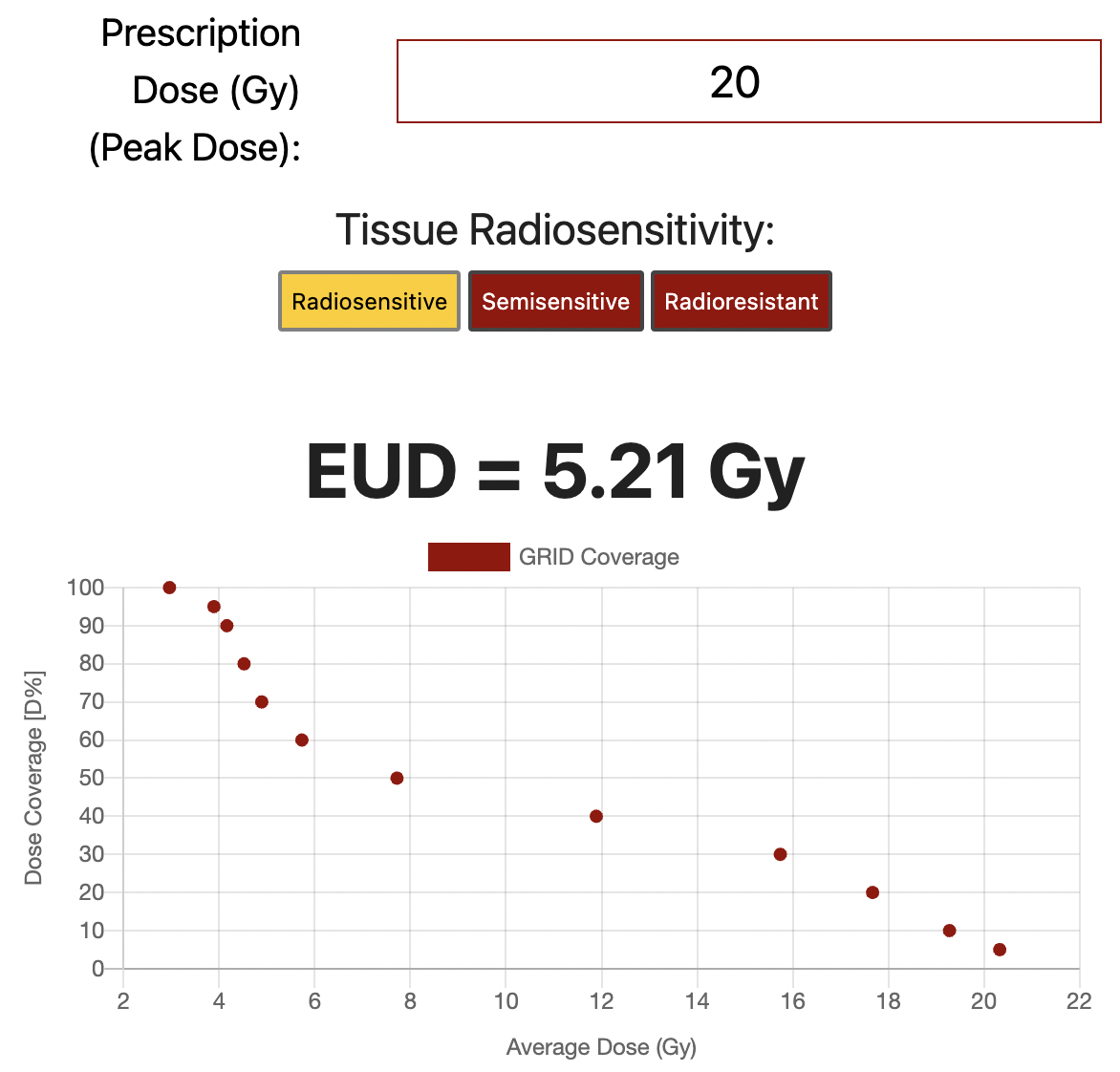
Dedicated to projects that improve the patient experience and medical predictions
Assistant Professor of Clinical Radiation Oncology
Director of Brachytherapy
- Affiliation: University of Southern California
- Website: drandrewlim.com
- Phone: (323) 865-3050
- Degree: MD, BSc
- Email: andrew.lim@med.usc.edu
- City: Los Angeles, USA
A diagnosis of cancer rightfully carries much anxiety and feelings of helplessness, but my philosophy is that there is always hope!
As a Radiation Oncologist, I listen to the needs of my patients, use my medical knowledge, and collaborate with my team of doctors, nurses, social workers, psychologists to create a plan that is tailored to my patient’s goals. Much anxiety is derived from feelings of helplessness, and that is why I believe that it is important that the patient be in control every step of the way.
Resume
Summary
Andrew Lim MD
Radiation Oncologist specializing in advanced Interventional Radiation Oncology (Brachytherapy). He is also an entrepreneur, dedicated to projects that improve the patient experience and medical predictions!
Specialities include Prostate Cancer, Gynecologic Cancers, Sarcomas, and metastatic cancers.
- USC Norris Comprehensive Cancer Center, Los Angeles, USA
- (323) 865-3050
- andrew.lim@med.usc.edu
Education
Interventional Radiation Oncology (Brachytherapy) Fellowship
2020 - 2021
University of California (UCLA), Los Angeles, CA
Radiation Oncology Residency
2016 - 2020
University of Alberta, Edmonton, Alberta, Canada
General Surgery Residency
2013 - 2016
University of Alberta, Edmonton, Alberta, Canada
Doctor of Medicine
2009 - 2013
Western University, London, Ontario, Canada
Bachelors of Science in Physics
2005 - 2009
St. Francis Xavier, Antigonish, Nova Scotia, Canada
Professional Experience
Assistant Professor of Clinical Radiation Oncology
Director of Brachytherapy
2022 - Present
University Of Southern California, Los Angeles, CA
- Leading the development of a world renowned Brachytherapy program at USC, with a focus on patient experience.
Radiation Oncologist
Assistant Professor
2021 - 2022
University Of Washington, Seattle, WA
- The development of a patient centered treatment for gynecologic cancers including Cervix cancer, Endometrial cancer, Vulvar cancer
Papers & Textbooks Chapters
Utility of machine learning of apparent diffusion coefficient (ADC) and T2-weighted (T2W) radiomic features in PI-RADS version 2.1 category 3 lesions to predict prostate cancer diagnosis
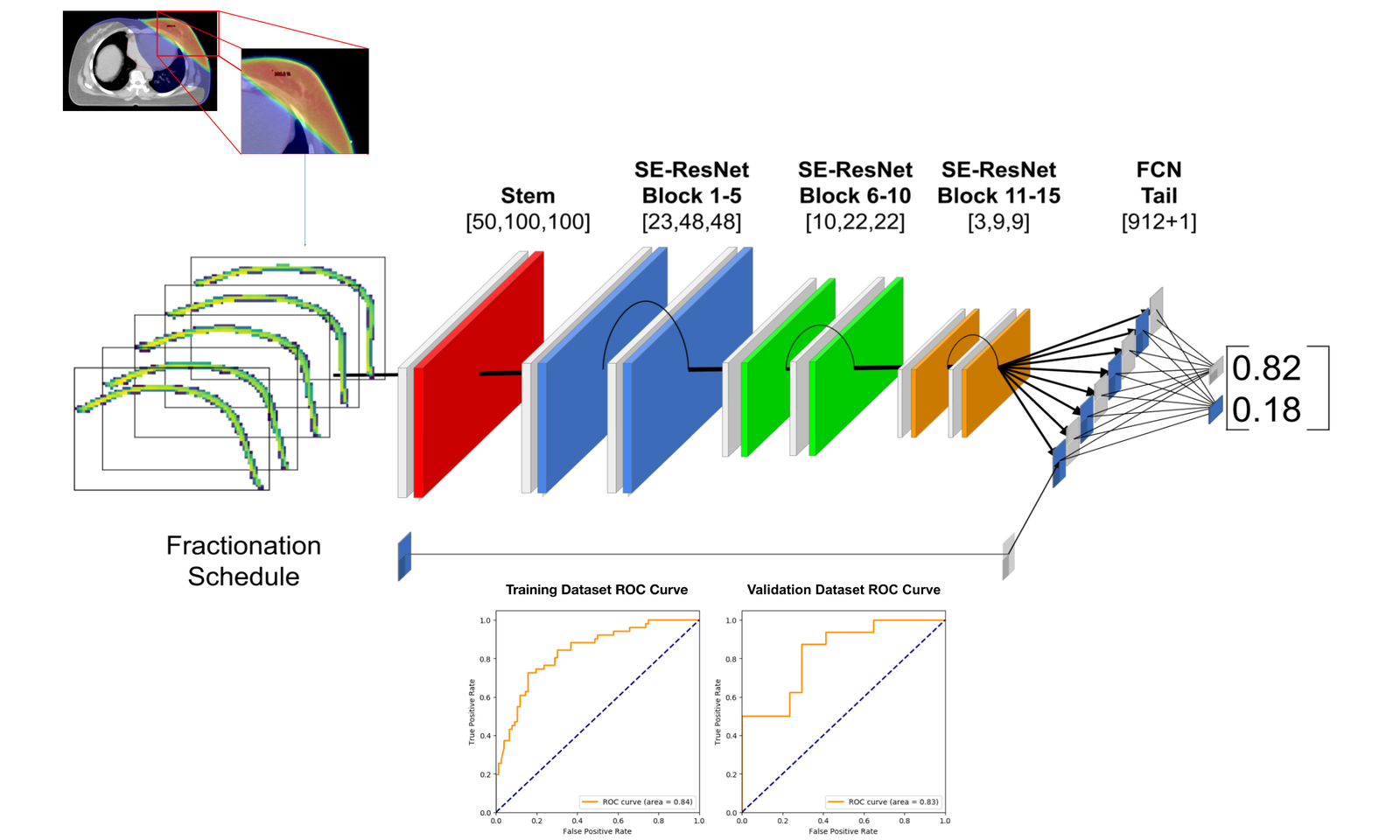
Purpose: To evaluate if machine learning (ML) of radiomic features extracted from apparent diffusion coefficient (ADC) and T2-weighted (T2W) MRI can predict prostate cancer (PCa) diagnosis in Prostate Imaging-Reporting and Data System (PI-RADS) version 2.1 category 3 lesions.
Results: From 160 PI-RADS 3 lesions, there were 50.0% (80/160) PCa, including 36.3% (29/80) CS-PCa (63.8% [51/80] ISUP 1, 23.8% [19/80] ISUP 2, 8.8% [7/80] ISUP 3, 3.8% [3/80] ISUP 4). The remaining 50.0% (80/160) lesions were benign. ML of all radiomic features from T2W and ADC achieved area under receiver operating characteristic curve (AUC) for diagnosis of (1) CS-PCa 0.547 (95% Confidence Intervals 0.510-0.584) for T2W and 0.684 (CI 0.652-0.715) for ADC and (2) any PCa 0.608 (CI 0.579-0.636) for T2W and 0.642 (CI 0.614-0.0.670) for ADC.
Conclusion: Our results indicate ML of radiomic features extracted from T2W and ADC achieved at best moderate accuracy for determining which PI-RADS category 3 lesions represent PCa.
A Novel Composite Biomarker Panel For Detection Of Early Stage Non-small Cell Lung Cancer
Purpose:To investigate a novel composite methodology of using targeted serum microRNAs (micro ribonucleic acid; miRNA) and urine metabolites for the accurate detection of early stage non-small cell lung cancer (NSCLC).
Results:The ROC analysis of miRNA expression yielded a sensitivity of 96.4% and a specificity of 88.2% for the detection of early stage NSCLC, with area under the curve (AUC) = 0.91 (CI 95%: 0.80-1.0). Relative urinary concentrations of 4-methoxyphenylacetic acid (4MPLA) were significantly different between NSCLC and healthy control (p=0.008). The ROC analysis of 4MPLA yielded a sensitivity of 82.1% and a specificity of 88.2%, with AUC = 0.85. The composite process combining miRNA and metabolite expression demonstrated a sensitivity and specificity of nearly 100% and AUC=1.
Conclusion:A highly specific, sensitive and non-invasive detection method for NSCLC was developed. Pending validation, this can potentially improve the early detection and, hence, the treatment and survival outcomes of patients.
Phyllodes Tumors-The Predictors and Detection of Recurrence
Purpose:Phyllodes tumors are rare breast neoplasms and the histopathological grade and surgical margins help guide treatment and follow-up. The traditional surgical teaching is resection with ≥10 mm margins, but are narrower surgical margins acceptable? The purpose of our study was to identify predictors of local recurrence.
Results:A total of 150 phyllodes tumors were included: 110 of 150 (73%) benign, 21 of 150 (14%) borderline, and 19 of 150 (13%) malignant. At initial surgery, 29 specimens had a positive margin and 15 (56%) underwent re-excision. Seventy tumors had a surgical margin of ≤1 mm, 40 had a margin of 2 to 9 mm, and 11 had a margin of ≥10 mm. There were 11 of 150 (7.3%) locally recurrent tumors: 5 of 11 (45%) benign, 3 of 11 (27%) borderline, and 3 of 11 (27%) malignant. In total, 10 of 11 locally recurrent tumors had a positive margin or ≤1 mm margin at initial surgery.
Conclusion:Phyllodes tumors can have a personalized treatment approach based on histopathological grade and surgical margins. Borderline and malignant phyllodes tumors with a positive or ≤1 mm surgical margin have an increased risk of recurrence. In benign phyllodes tumors, an optimal narrow negative margin may exist but the traditional ≥10 mm excisional margin is not necessary. Local recurrence rates may be sufficiently low in benign phyllodes tumors that imaging can be performed on the presence of clinical symptoms.
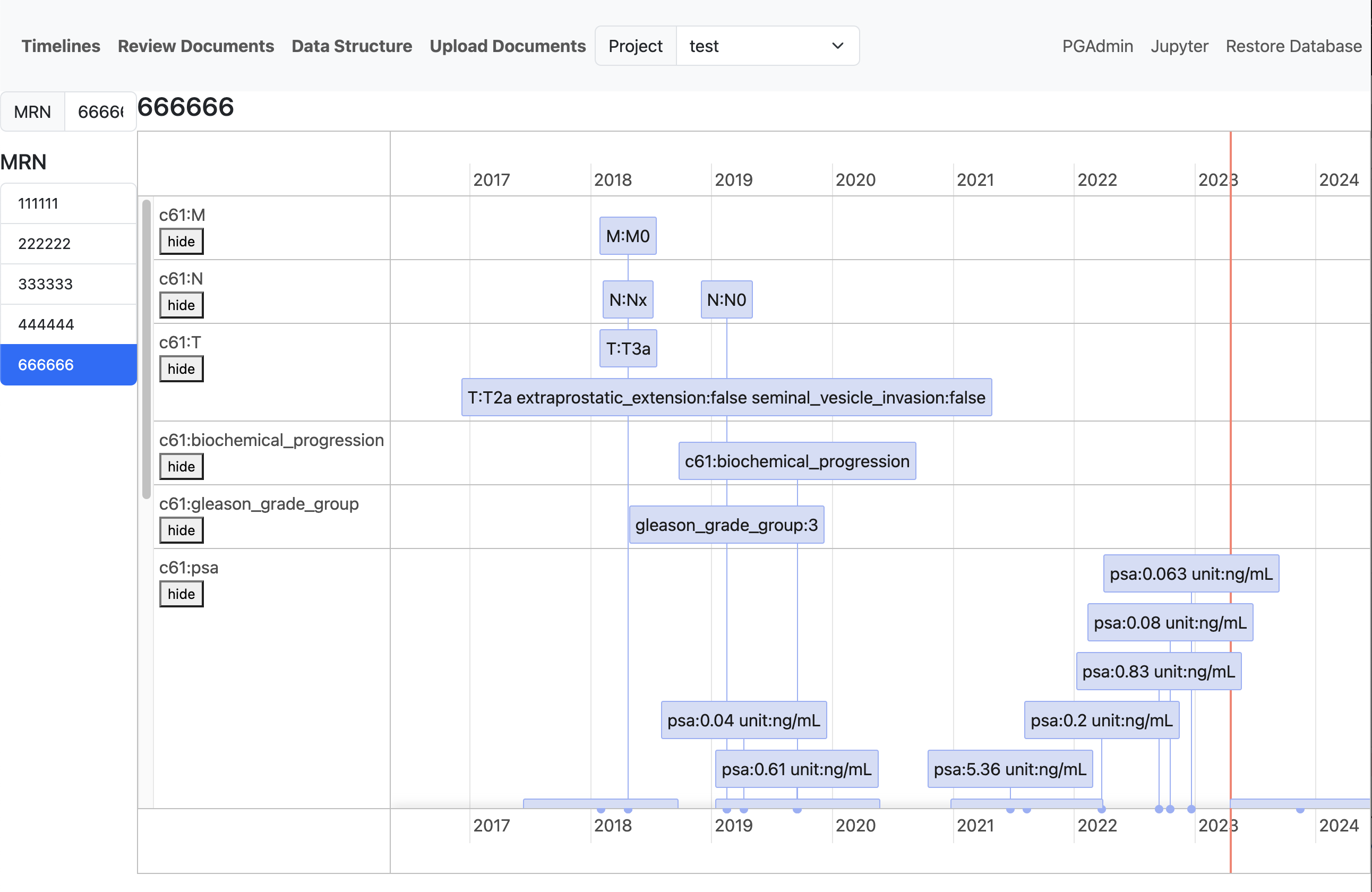
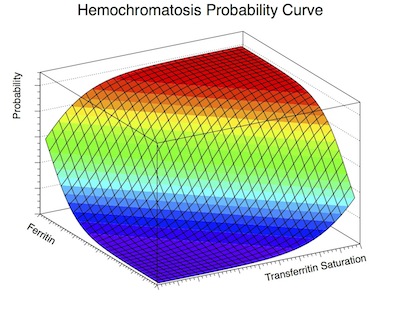
Predicting C282Y homozygote genotype for hemochromatosis using serum ferritin and transferrin saturation values from 44,809 participants of the HEIRS Study
Purpose:The simultaneous interpretation of serum ferritin level and transferrin saturation has been used as a clinical guide to diagnose genetic hemochromatosis. The Hemochromatosis and Iron Overload Screening (HEIRS) Study screened 101,168 North American participants for serum ferritin level and transferrin saturation, and C282Y genotyping for the HFE gene.
Results:The logistic equation had an area under the ROC curve of 0.91 for men and 0.89 for women. The pseudo R-squared was 0.44 for men and 0.34 for women. An example analysis was a Caucasian man with a transferrin saturation of 50% and a ferritin level of 500 µg/L, who had a 1.3% (95% CI 1.1% to 8.8%) probability of being a C282Y homozygote.
Conclusion:A large primary care-based sample of 44,809 participants contributed to the development of a new computer/smartphone tool that predicts the probability of being a C282Y homozygote of the HFE gene from serum ferritin and transferrin saturation values.
Khan’s Treatment Planning in Radiation Oncology:
Textbook Chapter: Cancer of the Genitourinary Tract: Prostate, Bladder, and Testicular Cancer.
Appendicitis: Risk factors, management strategies and clinical implications
Textbook Chapter: When Do NonOperative Management Strategies Outperform the Surgical Appendectomy?
Contact
Location:
USC Norris Comprehensive Cancer Center, 1441 Eastlake Ave, Los Angeles, CA 90033
Email:
andrew.lim@med.usc.edu
Call:
(323) 865-3000